The world’s first human graphene-based brain surgery procedure has been performed in Manchester.
INBRAIN Neuroelectronics said the procedure at Salford Royal Hospital saw its cortical interface used in a patient undergoing brain tumour resection.
Its technology was able to differentiate between healthy and cancerous brain tissue with micrometre-scale precision, the company claimed.
This milestone represents a significant advancement in demonstrating the ability of graphene-based BCI technology beyond decoding and translating brain signals, to become a reliable tool for use in precision surgery in diseases such as cancer, and in neurotechnology more broadly.
The study was sponsored by the University of Manchester, and primarily funded by the European Commission’s Graphene Flagship project. It was led by chief clinical investigator Dr David Coope, a neurosurgeon at the Manchester Centre for Clinical Neuroscience and brain tumours theme lead at the Geoffrey Jefferson Brain Research Centre, and chief scientific investigator Kostas Kostarelos, professor of nanomedicine at the University of Manchester, the Catalan Institute of Nanoscience & Nanotechnology, and co-founder of INBRAIN.
“The world’s first human application of a graphene-based BCI highlights the transformative impact of graphene-based neural technologies in medicine. This clinical milestone opens a new era for BCI technology, paving the way for advancements in both neural decoding and its application as a therapeutic intervention,” said Carolina Aguilar, CEO and co-founder of INBRAIN.
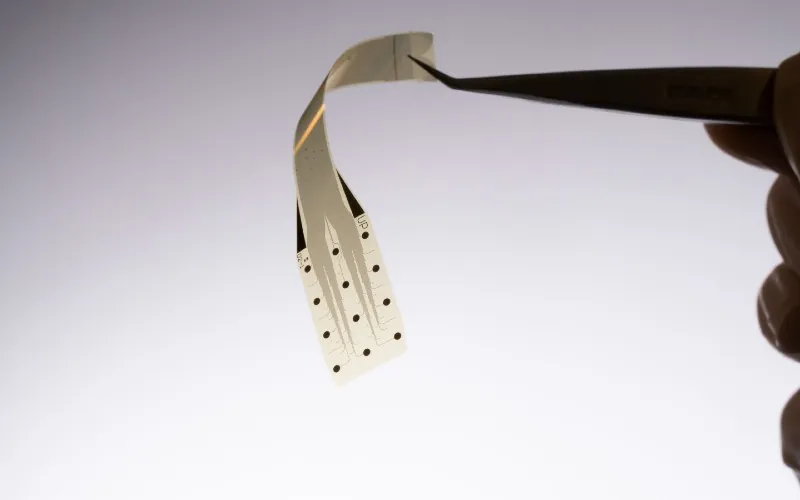
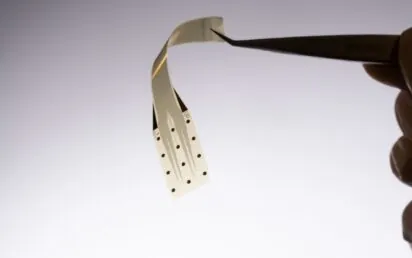
INBRAIN’s BCI platform leverages the exceptional properties of graphene, a material made of a single layer of carbon atoms. Despite being the thinnest known material to science, graphene is stronger than steel and possesses a unique combination of electronic and mechanical properties that make it ideal for neurotechnology innovation.
“We are capturing brain activity in areas where traditional metals and materials struggle with signal fidelity. Graphene provides ultra-high density for sensing and stimulating, which is critical to conduct high precision resections while preserving the patient’s functional capacities, such as movement, language or cognition,” said Dr Coope, the neurosurgeon who performed the procedure.
Kostarelos added: “After extensive engineering development and pre-clinical trials, INBRAIN’s first-in-human study will involve 8-10 patients, primarily to demonstrate the safety of graphene in direct contact with the human brain.
“The study will also aim to demonstrate graphene’s superiority over other materials in decoding brain functionality in both awake and asleep states.”